Clinical Curriculum
Our curriculum continues to evolve as we identify innovative pathways to enhance academic growth and strenghten the clinical experience. Most recently we have added a community-ED rotation (at Cooperman Barnabas Medical Center in Livingston, NJ) as well as expanded our offerings in sub-specialty areas as we focus on training the next generation of emergency physicians in innovative and effective ways. The outline below reflects the curriculum as it is being implemented beginning July 2023 for the Class of 2027. Minor variation exist for residents that have already begun training.
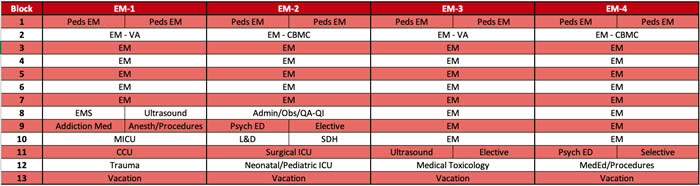
Each of our four years is divided into thirteen, four-week rotation blocks as follows (rotations do not occur in the sequence below) - the same information can be accessed in a more user-friendly format at: https://brickcityem.org
All EM blocks include approximately 10% Pediatric ED shifts and daily exposure to Psychiatric ED patients
Block Descriptions:
EM-1
Introduction to Emergency Medicine - 1 block
All incoming first-year residents begin their residency in July in the Emergency Department (ED) at University Hospital (UH). There is extra resident coverage in the ED during this month to allow an easier transition for first-year residents. The number of shifts worked are reduced to make room for an integrated EM Boot Camp which teaches basic core concepts in Emergency Medicine through lecture, small group sessions, skills workshops and simulation exercises.
Emergency Medicine (University Hospital) - 4 blocks
As a first-year resident, time spent in the ED is geared toward establishing a foundation of Emergency Medicine’s core concepts. The primary goals are to learn how to work up the basic chief complaints seen in the ED and learn to differentiate between the “sick” and “not sick” patient. Firstyear residents are encouraged and expected from day one to perform any and all procedures in the department including intubation, chest tube insertion, central line insertion, lumbar puncture, and laceration repair. These procedures are supervised by a senior resident or attending. Approximately 1-2 shifts during each block are spent in the Pediatric ED at UH, giving residents exposure to the variety of pediatric pathology spread across the calendar year. Residents will also spend approximately 1-2 shifts/block in the Fast Track area of the ED beginning August 2017.
Emergency Medicine (East Orange VA Hospital) - 1 block
This rotation affords the first-year resident an opportunity to learn and practice the basics of emergeny medicine in a smaller, community-based ED setting with one-on-one supervision from an attending physician. This experience also adds in some Fast Track experience so that residents become comfortable with bread-and-butter/basic EM pathology.
Pediatric Emergency Medicine - 1 block
This rotation is divided into two 2-week blocks, ideally one in warmer months and one in colder months so that residents gain exposure to the seasonal variation in pediatric pathology. The rotation is based at University Hospital's Pediatric ED, with primary supervision of residents provided by Pediatric EM-trained faculty.
Ultrasound - 0.5 block
Utilization of ultrasound in EM continues to grow and it is a core tool in our ED. During this dedicated two-week rotation, first-year residents learn how to use the ultrasound machine at a basic level on patients in the department - the physics of ultrasound, “knobology”, how to best capture and save images, etc. Upon completion residents are expected to have competence in using the ultrasound for procedures, along with exposure to key emergency studies. The first-year resident is paired with a senior resident for the rotation, and is overseen by our ultrasound faculty.
Emergency Medical Services (EMS) - 0.5 block
One week of this block is spent on the ground doing shifts alongside paramedics and EMTs in the ambulance as they evaluate and transport patients around Newark to various hospitals in the area. The other week is spent with NorthSTAR (Shock-Trauma Air Rescue). Flying on the helicopter for medical evacuations with flight nurses and paramedics is an optional experience.
Addiction Medicine - 0.5 block
During this rotation residents work faculty from both the Department of Emergency Medicine and the Department of Psychiatry as they evaluate and manage patients with a variety of addictions and substance abuse in both the inpatient, emergency and outpatient setting. This rotation allows residents to work directly with renowned experts in the field and participate in grant-funded research projects, while directly impacting our patients given the high rate of substance abuse and addiction in the Newark area. Resident also spend time in the CARE center and work with CARE navigators focused on medication-assisted treatment and outpatient transitions of care. This experience provides residents with focused education in an area of continued future need and importantly beyond the basic exposure obtained during routine ED shifts.
Anesthesia (AM)/Procedures (PM) - 0.5 block
This block combines Anesthesiology in the morning along with Procedures in the afternoon. The Anesthesiology rotation provides first-year residents the opportunity to learn to manage the airway in a controlled Operating Room setting using a variety of modalities - BVM ventilation, direct and video-assisted laryngoscopy, LMA, etc..
While on the Procedures rotation residents focus on ED-based procedures while also working alongside a variety of consultants in learning procedural skills relevant to the acute management of ED patients. While on this rotation the resident fields consults from the ED related to a variety of specialties such as Orthopedic Surgery, Plastic Surgery, Ophthalmology, Otolaryngology, etc.. The resident works as a liaison and partner with the consulting service while learning and performing key procedures including fracture reductions, complex laceration repair and ophthalmologic procedures.
MICU - 1 block
While on the Medical Intensive Care Unit, first-year residents serve a primary role as part of the critical care team. The team is composed of ICU attendings, fellows, residents from multiple specialties and medical students. This rotation is a great setting to manage the sickest patients over their disease course. By the end of this rotation, first-year residents are comfortable treating conditions such as DKA, severe sepsis/septic shock, massive GI bleeding, and strokes. They also gain competence in placing central lines, managing a ventilator, and selecting/dosing vasopressors.
CCU - 1 block
While on the Coronary Care Unit, first-year residents serve a primary role as part of the Cardiology critical care team. The team is composed of Cardiology attendings, fellows, Internal Medicine residents, and medical students. This rotation particularly exposes residents to the management of very common, but life-threatening cardiac conditions such as congestive heart failure, myocardial infarction, and heart block. This allows for focused exposure to echocardiography, cardiac catheterization, pericardial windows, and pacemakers, among other things.
Trauma - 1 block
As northern New Jersey’s only level-1 trauma center, UH is a prime location for great trauma exposure including high speed motor vehicle accidents, falls from high elevation, burns, stab wounds, and gunshot wounds. Almost one-third of trauma activations are for penetrating injuries (significantly higher than comparable national trauma centers) and our Injury Severity Score for trauma activations is higher than our peer group of trauma centers. This dedicated rotation allows first-year residents to be part of the Trauma Team that responds to Priority 1 and 2 trauma activations in the ED, and care for the inpatient service. The team is composed of attending physicians, fellows, residents from various specialties, nurse practitioners and medical students. First-year residents perform primary and secondary surveys, FAST ultrasound examinations, and place chest tubes and central lines. Resuscitative thoracotomies are frequently performed in the ED Trauma-Shock Room. Trauma is also integrated within EM blocks during EM-3 and EM-4 years.
EM-2
Emergency Medicine (University Hospital) - 5 blocks
Second-year residents become more well-rounded, efficient, and complete in their work-up of patients. Often during this year, residents work one-on-one with an attending on the "low side" managing upwards of 10-15 patients at a time. By the end of second year, residents feel confident in their multi-tasking ability and are able to manage most patients on the non-trauma side independently (with attending supervision). Furthermore, residents are now expected to take presentations from medical students, and learn to balance clinical and teaching responsibilities with regard to students. Pediatric ED and Fast Track shifts continue to be scattered throughout each ED block.
Emergency Medicine (Cooperman Barnabas Medical Center) - 1 block
This rotation provides the second-year resident with exposure to a large, suburban community-based ED working in multi-disciplinary teams as well as a non-academic health center focus on patient flow and satisfaction.
Pediatric Emergency Medicine - 1 block
This rotation is divided into two 2-week blocks, ideally one in warmer months and one in colder months so that residents gain exposure to the seasonal variation in pediatric pathology. The rotation is based at University Hospital's Pediatric ED, with primary supervision of residents provided by Pediatric EM-trained faculty.
Emergency Psychiatry - 0.5 block
During this rotation residents work faculty and residents from the Department of Psychiatry in the psychiatric section of the Emergency Department. Residents gain skills related to the evaluation of patients presenting with acute psychiatric conditions, psychiatric clearance and management of substance-induced psychiatric disorders. With the growing national crisis related to mental health and lack of adequate psychiatric inpatient beds this rotation introduces residents to a core area of future emergency medicine practice.
ED Administration/QA-QI & Observation Medicine - 1 block
This rotation provides exposure to principles of ED administration, including managing patient flow, throughput, physician scheduling, research management, and collaboration with other departments and institutional leadership. During their Observation Medicine shifts residents are exposed to an EM-managed protocol-driven observation unit. They further develop clinical skills in assessment, treatment and discharge planning, while learning to oordinate care plans with other physician and healthcare providers. Finally, the rotation affords residents time to develop and conduct an individual quality assurance/quality improvement (QA/QI) project - over the past few years 100% of these projects have been accepted as abstracts to the annual SAEM meeting.
Social Determinants of Health/Community & Urban Health - 0.5 block
Newark is a significantly underserved area with significant socio-economic challenges. To be effective in the care of our ED patients we need to understand them and the resources available (or not available) to them. This novel rotation is designed to expose residents to the circumstances in which our patients reside and seek healthcare. Residents will work with an inter-disciplinary team including students (health-related professions, medicine, nursing and public health), nurses, nurse practitioners and community health workers, with supervision from EM faculty involved in Community/Urban Health. Residents will be introduced to the complex problems of health care delivery to marginalized and underserved populations, along with affording them an opportunity to improve their skills in cultural competency, community empowerment and interdisciplinary communication.
Obstetrics & Gynecology - 0.5 block
This block is focused on Labor & Delivery and residents gain comfort with the assessment and management of patients beyond 20 weeks in their pregnancy.
During this rotation on the Labor & Delivery Unit of UH, residents are exposed to a variety of common Ob/Gyn emergencies and perform supervised vaginal deliveries in a controlled setting.
SICU - 1 block
The Surgical Intensive Care Unit is often an extension of the trauma bay at University Hospital. As a result, these are often the sickest patients in the hospital. This is also an opportunity to manage high-risk and complicated post-operative patients. While on this service, residents further learn to manage ventilators, are exposed to tracheostomy placement, manage and place chest tubes, and manage and place central lines. The team consists of surgical residents, EM residents from other institutions, trauma fellows, and trauma attendings.
N/PICU - 1 block
During this joint Neonatal and Pediatric Intensive Care Unit rotation, residents are part of a team managing critically ill neonates and pediatric patients in the hospital. They perform neonatal resuscitations during high-risk obstetric deliveries, often being the senior resident on the team. After the deliverys, many of these patients are on ventilators and multiple medication infusions. This rotation also allows a focused environment for performing procedures on pediatric patients including intubation and lumbar puncture.
Elective - 0.5 block
This block is designed to allow residents to explore their clinical, scholarly and/or research interests whether related to future career/fellowship plans or purely their clinical interests. By affording them elective time early in residency it allows residents to "try" experiences they may not otherwise consider.
EM-3
Emergency Medicine (University Hospital) - 8 blocks
The expectation of a third-year resident is to become comfortable managing the entire "high-side" of the department, now including trauma patients. Over the course of the year, faculty give third-year residents growing independence and supervisory responsibilities. Residents start to take presentations from junior residents, in addition to medical students, and help them make management decisions while providing teaching points. On the “high side” of the department, they simultaneously see patients coming through the Trauma Bay. In the Trauma Bay the ED team manages significant portions of patients independently. For the sickest trauma patients (Priority 1 & 2) the ED co-manages the patient with the Trauma Team, with the EM resident taking primary responsibility for airway management, while also assisting with the primary and secondary surveys, and management decisions. Pediatric ED and Fast Track shifts continue to be scattered throughout each ED block.
Emergency Medicine (East Orange VA Hospital) - 1 block
This rotation affords the third-year resident an opportunity to function as a junior attending in a smaller, community-based ED setting with one-on-one support from an attending physician. This experience also adds in some Fast Track experience so that residents become comfortable with bread-and-butter/basic EM pathology.
Pediatric Emergency Medicine - 1 block
This rotation is divided into two 2-week blocks, ideally one in warmer months and one in colder months so that residents gain exposure to the seasonal variation in pediatric pathology. The rotation is based at University Hospital's Pediatric ED, with primary supervision of residents provided by Pediatric EM-trained faculty.
Ultrasound - 0.5 block
The second-half of the formal ultrasound rotation occurs in third-year where the senior resident is coupled with a first-year resident. Residents work on advanced ultrasound skills including echocardiography, eFAST, etc. Additionally, they are responsible for teaching first-year residents basic ultrasound skills. The rotation is overseen by our ultrasound faculty with images being uploaded into our electronic medical record, stored and reviewed.
Medical Toxicology - 1 block
The NJ State Poison Center is located on our campus and is formally part of our Department of Emergency Medicine. This rotation allows residents to hear about, manage, and follow all reported poisonings throughout the state. Didactics are integrated throughout the rotation with lectures delivered by Toxicology fellowship-trained physicians. Residents routinely produce case reports and other publications related to toxicology during this block.
Elective – 0.75 blocks
This block is designed to allow residents to pursue their clinical, scholarly and/or research interests. They now have time to develop a scholarly project and implement portions of it longitudinally over the course of their residency. Furthermore, this allows the resident to build a portfolio that would strengthen their application for fellowships, jobs, etc. in a focused area of interest. Based on their specific interests the resident can also engage in an elective clinical rotation.
EM-4
Emergency Medicine (University Hospital) - 8 blocks
The fourth-year resident is expected to easily manage either side of the department independently (with available supervision), while also monitoring patient flow throughout the ED, and taking on significant supervisory and teaching responsibilities. There is greater emphasis on managing the whole team rather than simple seeing a large volume of patients individually. Residents continue managing trauma patients while on the “high side.” Students and junior residents on the team are expected to present their patients to the fourth-year resident, with the fourth-year guiding management decisions. Pediatric ED and Fast Track shifts continue to be scattered throughout each ED block.
Emergency Medicine (Cooperman Barnabas Medical Center) - 1 block
This rotation provides the fourth-year resident with key senior-level experience at a large, suburban community-based ED working in multi-disciplinary teams as well as a non-academic health center focus on patient flow and satisfaction. The fourth-year resident is expected to function in a pre-attending role with a significant focus on the upcoming transition to independent practice.
Pediatric Emergency Medicine - 1 block
This rotation is divided into two 2-week blocks, ideally one in warmer months and one in colder months so that residents gain exposure to the seasonal variation in pediatric pathology. The rotation is based at University Hospital's Pediatric ED, with primary supervision of residents provided by Pediatric EM-trained faculty.
Medical Education & Procedures- 1 block
Integrated within this block is a teaching rotation whereby residents spend time in the ED without primary patient care responsibilities, acting principally as an educator, taking student and resident presentations while providing salient learning points. Residents also work closely with our MedEd faculty to learn various aspects of Medical Education administration, while also serving in teaching roles for student didactics and simulation.
During this rotation residents also simultaneously participate in ED-based procedures while also working alongside a variety of consultants in learning procedural skills relevant to the acute management of ED patients. While on this rotation the resident fields consults from the ED related to a variety of specialties such as Orthopedic Surgery, Plastic Surgery, Ophthalmology, Otolaryngology, etc.. The resident works as a liaison and partner with the consulting service while learning and performing key procedures including fracture reductions, complex laceration repair and ophthalmologic procedures. This further reinforces their procedural training as they prepare to graduate from residency.
Selective - 0.5 block
This block allows senior residents to hone their clinical skills and prepare for their future practice by selecting from a shortlist of clinical rotations such as Regional Anesthesia, Electrophysiology, Sports Medicine, Palliative Care, etc.
