Surgical Simulation

Open and laparoscopic suturing, knot-tying, and instrument manipulation are basic technical diagnostic and therapeutic skills required for all trainees in general surgery, surgical subspecialties (Urology, ENT, Neurosurgery, Vascular, Colorectal, Trauma, etc.), and Obstetrics/Gynecology. The traditional model of surgical training is no longer viable due to increase in complexity of surgery, a plethora of newer surgical techniques, the regulatory demands on patient outcomes and patient safety, and the prioritization of patient comfort, all to be accomplished within the same time frame of training as almost a century ago , however, with new work hour limitations. Novices in surgery are significantly more likely to encounter complications, cause patient discomfort,and have a long procedure time than experienced surgeons for diagnostic and therapeutic procedures, all of which can lead to patient complications. In an era where mandates on patient safety, patient comfort, and patient outcomes must be balanced with increasing demands on resident education, procedural learning must occur in adjunctive environments, such as in the simulation lab and using virtual reality. High fidelity simulation environments and virtual-reality based surgical simulators offer several potential advantages over traditional surgical training: (1) interactive environment of teaching that uses effective adult learning principles; (2) computer graphics simulation uses computerized images displayed in response to the surgical skill being performed; (3) no procedure-related errors to patients can occur; and (4) the “novice” has now been pre-trained to safely perform procedures on patients with an improved educational learning curve. Clinical researchers have reported the following benefits of simulation training:
- Data has clearly shown a significant benefit to patient safety and improved patient outcomes when the initial part of technical skills training occurs in a safe, simulated environment without real patients.
- It allows repeated practice of standardized tasks and realistically complicated maneuvers until competency, without sacrificing patient safety and hospital resources.
- The skills training and assessment programs, developed by expert surgeons, are easy to administer and adhere to and meet high standards of reliability and validity, and can be used to assess technical proficiency in surgical skills prior to performing procedures on patients.
- They allow unbiased, objective, and reproducible assessments of surgical skill performance, leading towards proficiency standards.
- High-risk and high stress environments, such as surgical complications, trauma, and team crises can be replicated without the patient, leading to proficiency in these situations and contributing to improved patient outcomes.
- Trainees who learned in a simulated environment prior to performing procedures on patients had a much smaller learning curve when in the real clinical environment, and achieved proficiency much quicker.
- Almost every aspect of medical and surgical training, from operative techniques, trauma and resuscitation, error disclosure, and team-work, can be simulated.
 Fundamentals of Laparoscopic Surgery and Laparoscopic Simulation
Fundamentals of Laparoscopic Surgery and Laparoscopic Simulation
In addition to the above advantages and rationale, recently, the American Board of Surgery has required trainees to pass the surgical simulation assessments, known as Fundamentals of Laparoscopic Surgery (FLS) and Fundamentals of Endoscopic Surgery (FES), in order to be a Board Certified surgeon in the United States. Moreover, surgical training program accreditation now requires the presence of a comprehensive simulation curriculum for the residents. Successful completion of FLS, FES and FUSE and also successful implementation of a simulation curriculum, is predicated upon a proper practice environment to be provided by the trainee’s institution. Our practice environment includes equipment, resources, and a curriculum for successful training of our surgical residents:

A resident practicing endoscopic skills on colonoscopy simulation model.

Residents practicing skills for fundamentals of laparoscopic surgery.
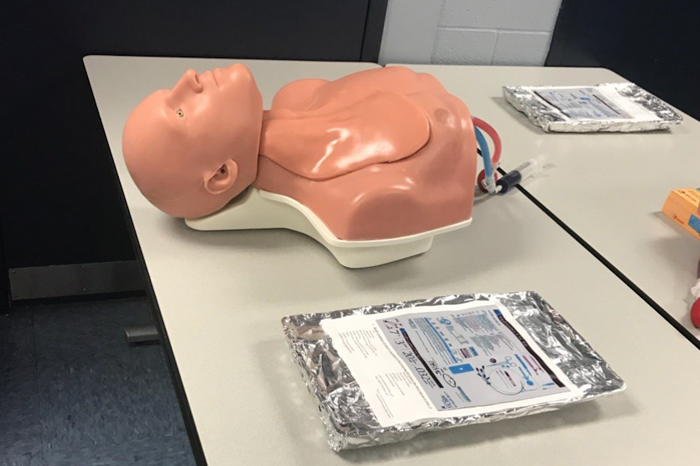
Mannequin used for practicing central line placements.

Residents performing bowel anastomoses.

Vasular surgeon Dr. Huang teaching residents vasular anastomoses.
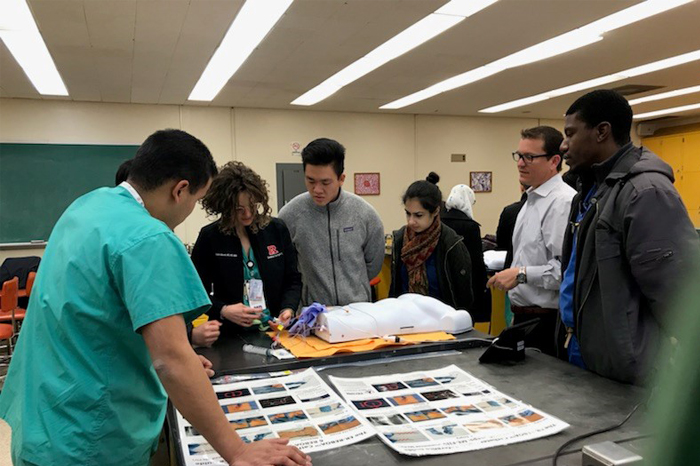
Intern residents reviewing landmarks for central line placement.

