Center for Immunity & Inflammation (CII)
The CII at Rutgers Health New Jersey Medical School Cancer Center is a multidisciplinary and highly collaborative center with laboratories dedicated to researching allergies; chronic autoimmune diseases like Crohn's disease, diabetes and lupus; fungal, protozoan, bacterial, viral, and helminth pathogens; pain management, sepsis, toxoplasmosiss, malaria, Vitamin D, and cancer. Research focuses on investigation of immunity in the context of these infectious and noninfectious diseases. Some of our most recent papers are shown below.
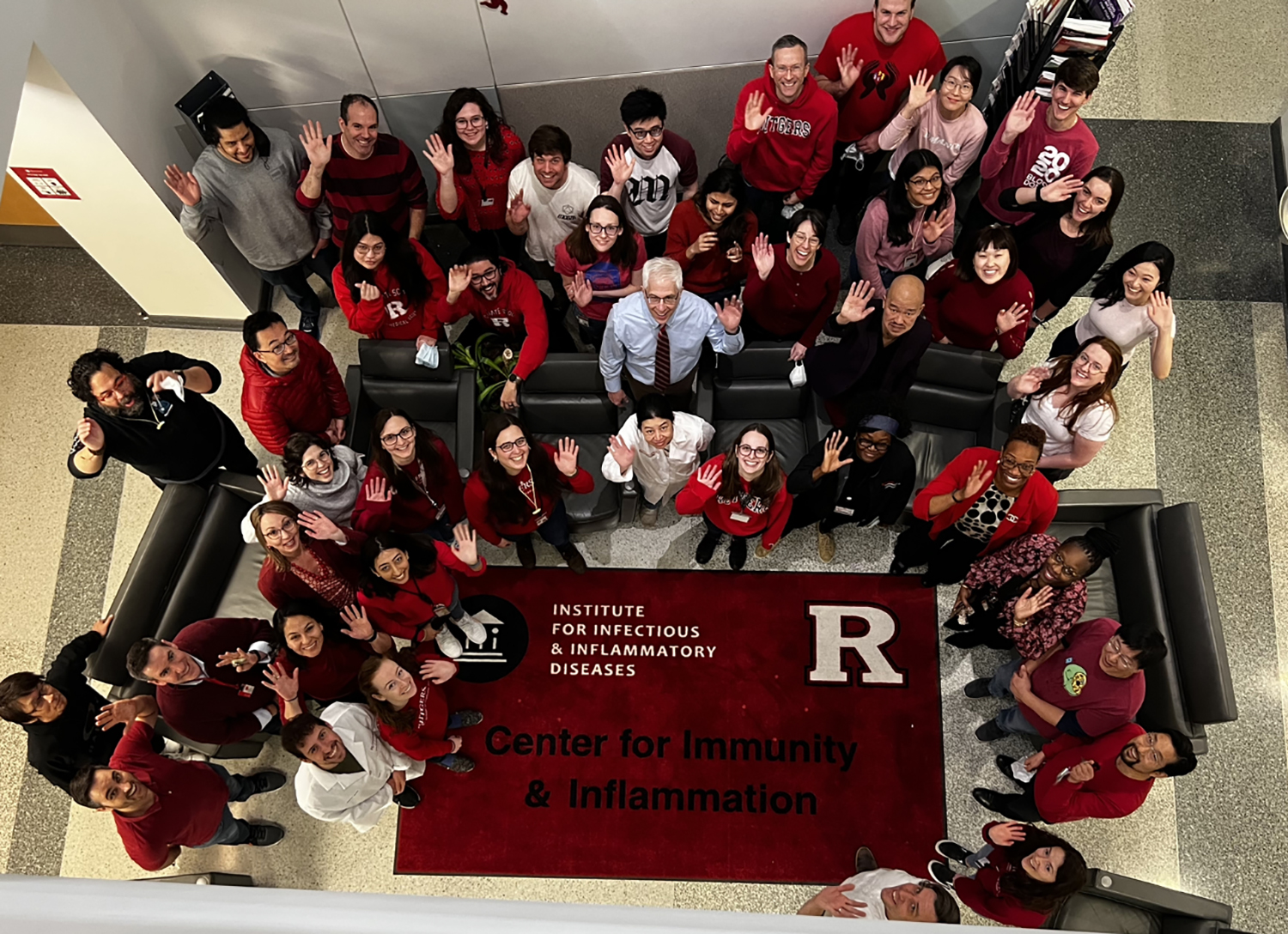
CII is highly interactive with faculty staff and students participating in a variety of activities including journal clubs and various center wide data clubs and more focused group lab meetings. Monthly seminars with outside speakers and annual internal retreats and symposia are held to facilitate interactions and potential collaborations.
CII members have access to nearby Core Facilities that include a Biostatistics Core; Center for Genome Informatics; Experimental Histology & Confocal Imaging Core; Flow Cytometry and Immunology Core Laboratory; and the Genome Editing Core among others.


Dr. William C. Gause
Director
Message from the Director
Fundamentally, the function of the immune system is to keep us healthy. It protects us from infectious pathogens, but it also plays a critical role in wound healing and tissue repair, and it plays an essential role in protecting us from cancer. Unfortunately, there is also a prominent dark side to the immune system. The very same armaments that protect us and keep us healthy can sometimes get out of control. In many infectious diseases, the actual damage to the tissue and resultant disease is largely caused by the immune system itself. For example, in COVID-19 our immune system contributes to lung injury, long COVID, and multisystem inflammatory syndrome (MIS). As such, in addition to new diagnostics, treatments that target the pathogens, and effective vaccines, we also need to develop targeted methods that control associated harmful inflammation. At CII, we have ongoing research investigating host protective and harmful immune responses to a variety of bacterial, viral, fungal, and parasitic pathogens.
In some cases, the immune system can even become activated and cause disease in the absence of an infectious agent. This can lead to a variety of immunologic disorders, many referred to as autoimmune disorders. In recent years the prevalence of these diseases has increased particularly in westernized, developed countries. Environmental factors that might be involved include: toxic chemicals, particulate pollution, dietary components, and gut dysbiosis. In addition, although there are currently partially effective treatments for these diseases, there are as yet no cures. At the CII we have outstanding NIH funded faculty conducting cutting-edge research in a number of these inflammatory and autoimmune diseases. These include gastrointestinal diseases such as Crohn’s disease and ulcerative colitis, with a strong interest in effects of the microbiome; rheumatoid diseases such as serum lupus erythematosus; neurological diseases including multiple sclerosis, diabetes, and lung associated diseases including asthma and allergies.
Since 2016 the Center for Immunity and Inflammation has grown dramatically, recruiting over two dozen faculty from academic institutions throughout the United States including Yale, MIT, Johns Hopkins, University of Pennsylvania, University of Wisconsin, Cornell University, and Columbia University. Our ability to recruit these outstanding researchers is testimony to the excellence of our program, which now includes the critical mass of outstanding biomedical researchers needed to perform the cutting-edge research leading to new treatments and cures for some of the most intractable diseases. When you consider that each of these faculty members is awarded often multiple NIH grants, hiring half a dozen to a dozen highly trained staff for their laboratory, you can see we are already making an impact here in Newark. Much of this research is based in Newark at New Jersey Medical School and it provides a basis for improved patient care and community outreach in our city. We are also proud that we have recently developed a pathway program for Newark-based high school and college students to conduct summer research projects in our best laboratories. We plan to continue to reach out and engage the Newark community in activities ranging from participation in clinical trials to pathways programs for high school and college students.
The CII is already a major resource for biomedical discovery. CII laboratories are collaborating to develop large multi-investigator projects focused on fundamental discoveries and their translation to new treatments and therapies. Faculty at CII are participating in ongoing extensive collaborations with Rutgers, Newark; Rutgers, Camden; New Jersey Institute of Technology (NJIT); and Princeton University. Our vision at CII is to develop breakthrough discoveries and novel more personalized treatments. It acts as a nucleus for growing health care research and biomedicine and serves as an engine for the development of new products and services for the biotech and health care industry in New Jersey and throughout the country. This includes new targeted treatments and cures for autoimmune diseases, allergies, and immunologic disorders associated with infections by specific pathogens. As the global immunology market is projected to grow from $92 billion in 2021 to $158.69 billion in 2029 (Fortune Business Insights), we are well poised to contribute to this market.
The CII is an integral part of the Institute for Infectious and Inflammatory Diseases (i3D) a Chancellor level institute on the Rutgers Health campus. Infection and Inflammation has been selected as a signature area of strategic development and the i3D is already poised to become a national leader in this specialized area.
Department Administrator: Jennifer Yaney
