LIVER DISEASE
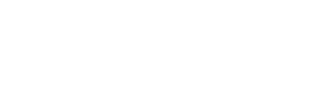
Normal Liver:
The liver is the largest solid organ in human body. It weighs about 1600 Gm in men and 1400 gm in women. It is a triangular or pyramid in shape and lies sideways in the upper right half of the abdomen with the base of the pyramid on the right side and the tip at the middle of the upper abdomen. Most of the liver is under the lower ribs and under normal conditions may not be felt by pressing on the abdomen except for its left portion that may be felt in the upper mid abdomen.
The gall bladder that stores bile, lies on its undersurface. The normal liver is brown in color, its surface is smooth band it is soft and pliable in texture.
Under Microscope:
The liver has well organized layers or plates of cells called liver cells. The cell plates are supported in a matrix of small amount of fibrillar scaffolding called connective tissue. The connective tissue usually accounts for 5-10% of normal liver weight. In addition the liver has smaller branches of blood vessels that supply and drain blood into and out of liver. It also has fine nerves and lymphatics.
As shown below liver cells are arranged as plates or cords of cells with collection of vessels at the center and at outer rim of the radiating liver cell cords.

Figure of normal liver as seen under microscope.
What does a normal Liver Do?:
- Acts as a filter for toxic substances and metabolizes various drugs and helps its elimination from the body.
- Makes various proteins, essential vitamins, hormones and chemicals for normal body function
- Makes bile and pours it out into the gall bladder that helps digestion
- Facilitates large number of metabolic processes of the body. It plays key role in the metabolism of carbohydrates, fat, and proteins.
- Makes various substances/factors that prevent excessive bleeding
Tests for Liver Disease:
Different tests are done to detect presence of liver disease. These tests can be put in three distinct categories:
- Tests to assess normal function of liver, also called Liver Function Tests or liver chemistry
- Tests that detect complications of liver disease that occurs as the liver disease progresses and becomes established and chronic.
- Tests specific for certain diseases and biopsy of liver.
Liver Function Tests:
These tests are based on normal functioning of liver. These tests essentially look for concentrations of certain elements or enzymes in the blood that are otherwise maintained within a tight range of normal values. When the liver does not function normally because of injury and disease the blood concentrations of theser substances deviate from their normal range. Most of the time these tests do not indicate the actual cause of the liver injury or disease, they only suggest that the liver is not functioning to its full normal capacity and is injured or is diseased. Identifying the cause of liver damage will probably require more definitive and specific tests.
Commonly used tests for liver function include the measurements of the following in the blood:
| Tests | Normal | If abnormal then indicates |
| Total Bilirubin | 0.2-1.0 mg% | Indicates Jaundice and severity of liver damage |
| Transaminase / Aminotransferase | ||
| ALT | 5-35 IU/L | Indicates liver cell injury |
| AST | 5-40 IU/L | Indicates Liver cell injury |
| Alkaline Phosphatase | 35-130 IU/L | Indicates poor ability to secrete bile and other Selective dysfunction |
| Albumin | 3.5-5.0 Gm% | Chronic liver disease |
| Prothombine time/INR | 12-15 sec/1.01 | acute liver injury |
Tests that detect complications of liver disease that sets-in as the liver disease progresses and becomes established and chronic:
These tests usually are complimentary to assess the gross appearance /distortion of liver, and presence of complications of liver disease. Examples are looking for nodular irregular liver, altered texture of the liver, abnormal varicose veins inside abdomen, collection of fluid in side the abdomen, enlargement of spleen and presence of liver tumor or cancer etc.
These tests are:
- Ultra sound imaging of liver
- CT scan of liver and abdomen
- MRI of Liver and abdomen
Tests specific for certain diseases and biopsy of liver:
There are specific tests to identify the cause of underlying liver disease. A thorough medical history, clinical examination of the patients give a clue to possible causev of the liver disease and then those tests are carried out to identify the causative agent.
Following are some of the specific tests foe the causes of liver diseases:
- Blood tests for Viral hepatitis A, B, C, Delta, E and other less common viral hepatitis.
- Hemochromatosis: A disease with abnormal storage of iron in liver and body
- Wilson's Disease: A disease characterized by accumulation of copper in liver
- Primary Biliary Cirrhosis (PBC)
- Primary Sclerosing Cholangitis (PSDC)
- Autoimmune hepatitis
- Other rare metabolic diseases of liver
- Liver Cancer: Screening test for alfa feto protein and imaging.
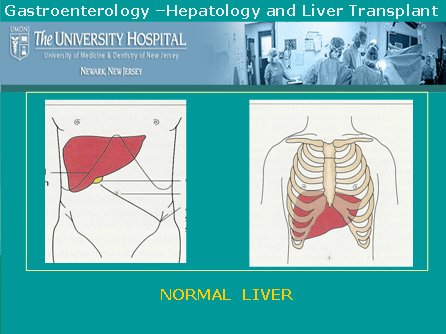
Liver Biopsy:
The process involves removing a tiny piece of liver by specialized needle and examining the tissue sample after proper processing and staining under a microscope. Patients are carefully selected to avoid and minimize risk of bleeding from the biopsy site. Biopsy is done either by approaching the liver in-between the ribs or through a vein in the neck and advancing a thin tubing (catheter guided biopsy needle) into the liver.

Figures: Liver Biopsy
Common Causes of Liver Disease:
Liver injury and liver disease can occur from a variety of causes. Various agents and disease conditions that commonly cause liver damage are the following:
- Viral infection (hepatitis A, B, C, Delta and E virus infections)
- Alcohol
- Obesity
- Complication of certain medications
- Abnormalities of hepatic veins: Budd-Chiary syndrome
- Exposure to chemicals
- Metabolic and genetic disorders
- Cancer
Symptoms and signs of Liver Disease:
Some of the signs and symptoms of liver disease include:
- Jaundice(Yellowing Of The Skin And Eye)
- Pruritus(Itching)
- Dark Or Tea-Colored Urine
- Muscle Wasting
- Skin may show "liver spots" , palm may be unduly bright mottled red
- Retention Of Fluid: This May Take The Form Of Ascites (Swelling Of The Abdomen With Fluid) And Or Swelling Of Ankles Or Legs With Fluid.
- Easy Bruising And Bleeding (Bleeding Gums Or Frequent Nosebleeds)
- Vomiting Blood
- Blood In The Stool (Bright Red Blood Or Black, Tar-Like Stool)
- Mental Confusion (Encephalopathy), sleep disturbance
- General feeling of ill-health: These are general symptoms not necessarily indicative of liver disease but reflect constitutional symptoms of poor health and illness in-general. These are fatigue, weight loss, debility, weakness, malaise, and poor appetite.
- In women: Menstural irregularity, infirtilty and early menopause are not uncommon with advanced liver disease.
- In men: decreased libido, erectile dysfunction, impotence, sterility, thinning of body hair and prominence of breast are seen with advanced liver disease.
Not every person with liver disease has all the above symptoms and signs. Manifestations of symptoms and signs are very variable. T one end of the wide spectrum of the disease an individual may not have any symptom despite the presence of established chronic liver disease and the diagnosis may be made following detection of abnormal blood tests at general health examination. On the other extreme a person may have most of the features described above and may be quite debilitated.
Liver Diseases and Conditions:
I. Cirrhosis
Continued or chronic injury to liver damages the liver cells. The damaged liver cells are replaced by scar tissue. Over time, the build-up of scar tissue becomes so great that it impacts blood flow through the liver, destroying more liver cells and ultimately leading to greater and greater loss of liver function – a condition called cirrhosis.
Causes of Cirrhosis:
Alcohol remains the most common cause of cirrhosis of liver. Other causes include chronic hepatitis C virus and hepatitis B virus infection, autoimmune liver diseases (autoimmune hepatitis, Primary biliary cirrhosis, primary sclerosing cholangitis), abnormal deposition of iron (Hemochromatosis), or copper (Wilson's Disease), exposure to drugs and toxins and other genetically inherited diseases like Cystic fibrosis and Alfa 1-antitrypsin Deficiency.
Symptoms and Signs of Cirrhosis:
As cirrhosis evolves patients develop various signs and symptoms of liver disease namely jaundice (yellowing of the skin and eye), pruritus (itching), dark, tea-colored urine, weight loss, muscle wasting, fatigue, ascites (swelling of the abdomen with fluid), easy bruising and bleeding (bleeding gums or frequent nosebleeds), vomiting blood, blood in the stool (bright red blood or black, tar-like stool), and mental confusion (encephalopathy). Cirrhosis of any cause increases the risk of developing liver cancer.
Not all these features may be present at any given time but may evolve as the disease progresses.
Diagnosis:
Presence of features mentioned above helps physicians to strongly suspect the diagnosis of cirrhosis. This can be further supported by blood tests, imaging the liver by ultrasound or CT scan and in instances by a liver biopsy. Liver biopsy is a test where a thin core of liver tissue is removed from the liver by inserting a thin needle into the liver after anesthetizing the skin of the right-lower chest. The tissue sample is examined under microscope.
II. Hepatitis:
Inflammation of liver is called hepatitis. The liver can get inflamed (sore) by a number of injurious things like: viruses (viral hepatitis), alcohol (alcoholic hepatitis), too much of fat accumulation in liver (non alcoholic steato hepatitis or NASH), deranged immune mechanism (autoimmune hepatitis), drugs, chemicals and toxins (toxic hepatitis) etc.
Different types of Hepatitis:
1. Viral hepatitis:
Commonly seen viruses that infect the liver causing hepatitis are named as Hepatitis virus A, Hepatitis virus B, and Hepatitis virus C. Other viruses that can cause hepatitis include hepatitis virus D, hepatitis virus E, hepatitis virus G, infectious mono virus and CMV.
Viral hepatitis is a major public health issue and remains the most common cause of liver disease world wide. In the USA over 300,000 get acute hepatitis due to one or the other viral infections. Over 15,000 Americans die each year from complications of chronic viral hepatitis and is estimated that in the next two decades annual death rate from all viral hepatitis together will be around 25,000.
Different types of viral hepatitis are given below:
i. Hepatitis A:
This used to be called infectious hepatitis. Infection occurs through contaminated food or water. Contaminated water, ice, uncooked contaminated food, uncooked shellfish (oysters, clams, mussels) are not an uncommon source of infection. It is estimated that annually around 75,000 cases of acute hepatitis A occur in USA .
Persons at risk: International travelers, institutions where prolong close person to person contact occurs (army camps, institutions, schools, day care centers), homosexuals.
Outcome after infection with hepatitis A virus: Acute hepatitis A occurs that almost always resolves. It never becomes smoldering disease or chronic hepatitis. Rarely, in 0.3% cases it result in acute liver failure requiring a liver transplant.
Common manifestations of acute hepatitis A is loss of appetite, fatigue, dark urine, nausea, headache, mild abdominal pain and low grade self limiting fever. Jaundice (yellowness of eyes and skin) may or may not occur. During acute stage of hepatitis patient's blood and bodysecretions are infectious to others.
Diagnosis is confirmed by special blood tests.
Vaccine is available to prevent the occurrence of this disease.
ii. Hepatitis B:
Infection occurs by contaminated needle, contaminated body piercing and tattooing equipments or sexual contact. Infants born to mothers with chronic hepatitis get infected during child birth or early infancy in about 90% of the cases.
It is estimated that word wide more there are more than 400 million and in USA over 1.25 million chronic carriers of the disease. Globally the disease accounts for 250,000 and in the USA 5,000 to 6,000 hepatitis B related deaths each year.
Persons at risk: Sexual transmission accounts for 1/3 of hepatitis B infection in USA . Other risk groups include intravenous drug users, people with hepatitis B infected person's household, residents of nursing homes, hemodialysis and hemophilia patients, prison and prison workers. Other persons at risk are healthcare workers, particularly those exposed to accidental cuts and bruises and hemodialysis staff.
Outcome after infection with hepatitis B virus: Acute hepatitis B occurs following infection. Three things may happen thereafter:
Acute hepatitis may slowly resolve with in six months without any chronic disease. This happens in about 90-93% of acute hepatitis B in adults and 50% of children with acute hepatitis B.
• Chronic hepatitis B infection with continued smoldering liver injury may result. This slowly progresses to scarring of liver and cirrhosis.
• Carrier of hepatitis without progressive disease.
These patients have no symptoms and usually do not have continued liver injury. However, they may be still infective and pass infection to others.
Acute infection with hepatitis B virus manifests with is loss of appetite, fatigue, dark urine, nausea, headache, mild abdominal pain and low grade fever and Jaundice (yellowness of eyes and skin). At times, acute hepatitis may not have any symptoms and go undetected. In about 10% of cases this becomes chronic smoldering infection with slow but continued liver injury leading to cirrhosis. It is estimated that there are about 1.25 million chronic carriers of hepatitis B in the USA . Risk of liver cancer is increased in patients with chronic hepatitis B. Alcohol use increases the progress of liver disease in hepatitis B
Diagnosis is made by special blood tests.
Vaccine is available that prevents the occurrence of the disease.
iii. Hepatitis C:
This hepatitis was called non-A non-B hepatitis. Infection commonly occurs through sharing intravenous drug use paraphernalia, body piercing or tattooing equipments or sexual contacts. Because of current screening of blood donors, now a days blood transfusion is not a source of hepatitis C infection.
The hepatitis C virus, discovered in 1989, is transmitted via blood, so anyone who had a blood transfusion before 1992 or has the above mentioned predisposition is at risk of developing hepatitis C. It's possible for an infected mother to pass along the virus to her child at birth. Researchers aren't sure whether hepatitis C can be transmitted sexually. If so, it's a rare occurrence, but people who've had multiple partners are encouraged to be tested for the virus.
World wide over 100 million and in the USA over 4 million people have are infected with hepatitis C virus. It is the leading cause of chronic liver disease. The hepatitis C virus kills between 10,000 and 12,000 Americans each year. The hepatitis C virus infection is by far the leading indication for liver transplantation in the United States, accounting for between 30% and 50% of liver transplants, depending on the state where the patient lives
Persons at risk: Blood transfusion prior to late 1992, intravenous drug users, patients on hemodialysis and hemophilia patients, body piercing and tattoo, military veterans who served in Vietnam, prisoners, homeless and people with HIV.
Outcome after infection with hepatitis C: Acute hepatitis C occurs following infection. It becomes a smoldering disease with slow but progressive injury or chronic hepatitis in 80-85% of cases. Chronic hepatitis C progresses to cirrhosis over an extended period of 20-25 years in about 25% patient.
Acute infection with hepatitis C virus mostly remains undiagnosed because patients usually do not have any symptoms. In about 1/3 of those who do get symptoms they are mild and do not interfere with daily activity. Patients may have loss of appetite, common- cold like symptoms with fatigue, lethargy, body-ache, and headache. Usually they do not have Jaundice (yellowness of eyes and skin).
Chronic hepatitis C occurs in about 80-85% of those who have had acute infection in the past. In most patients there are no symptoms and the diagnosis is made at routine blood test when liver enzymes are incidentally found to be increased leading to test for and detection of hepatitis C virus. Usual symptoms are fatigue, dull pain in upper part of abdomen on right side. In about 25% of patients with chronic hepatitis C the disease progresses to cirrhosis in about 20-25 years. Risk of liver cancer is increased in patients with chronic hepatitis C. Alcohol use increases the liver disease in hepatitis C.
Diagnosis is made by special blood tests.
No vaccine is currently available for hepatitis C.
2. Alcoholic Hepatitis:
Alcohol can cause inflammation of liver (hepatitis). It occurs in both heavy drinkers as well as in binge drinkers. This is described in subsequqent pages under alcoholic liver disease.
3. Autoimmune hepatitis: Autoimmune Hepatitis: Autoimmune Hepatitis:
This is a condition wherein one's immune system starts attacking their own organs, as if they did not belong to that individual. Autoimmune hepatitis primarily affects women and starts as early as adolescence. As the name suggests, autoimmune hepatitis can cause inflammation of the liver and other symptoms common to liver disease such as jaundice and itching as well as some associated with autoimmune disorders, namely, aching joints. Fatigue, common to both, is a frequently reported symptom. Lab tests show the presence of increased gamma globulin and smooth muscle antibodies in the blood.
Many people with autoimmune hepatitis respond well to prednisone treatment, which can relieve symptoms and cause elevated liver enzyme levels to return to normal. Autoimmune hepatitis is a condition that needs monitoring over the long term, as it can lead to cirrhosis and ultimately, the need for a liver transplant.
4. Toxic hepatitis:
Rarely, medications intended to help patients can cause the liver to become inflamed causing toxic hepatitis. In an occupational setting, toxic hepatitis can occur when workers are exposed to certain chemicals in a confined space and are not wearing or properly using respiratory protective gear. Other causes include certain medications, mushroom poisoning etc.
Mushroom
poisoning : Eating wild mushrooms can make a person severely ill,
or in the worst-case scenario, cause a painful death. One particular
type of mushroom, the Amanita phalloides causes about 90 percent of
all mushroom eating-related deaths. Mushroom poisoning typically involves
a latent period of as long as 24 hours, when no symptoms are felt,
followed by extreme gastrointestinal upset; damage to several organs,
including the liver; heart failure; seizures; and coma.
The mushrooms' toxins can have an especially severe effect on the
liver, attacking the organ's cells and shutting down some of its key
functions. When the liver begins to fail but there is medical reason
to believe the patient could survive the poisoning, that person may
be a candidate for liver transplantation.
III. Obesity and Liver Disease; Non-alcoholic fatty liver disease (NAFLD) and Non-alcoholic steatohepatitis (NASH);
Consumption of alcohol is the most common cause of accumulation of excess fat in the liver. It is now recognized that similar fat accumulation in the little alcohol. This is known as non-alcoholic fatty liver disease (NAFLD). While in most of such cases the fatty liver is from obesity and the liver continues to function well and may not present a problem during their lifetime. However, in some obese patients excess fat causes inflammation in the liver known as Non-alcoholic steatohepatitis ( NASH). NASH, in some patients, may cause progressive liver injury resulting ultimately in cirrhosis and other complications of liver failure including liver cancer.
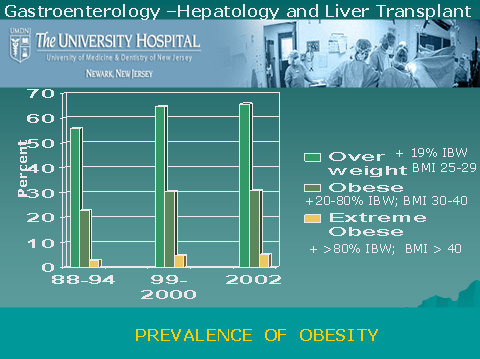
How Common Is Obesity Related Fatty Liver Disease:
Best estimates of prevalence of NAFLD are 18-20% and that of NASH is 4% in the general population. The prevalence of NASH increases with obesity and may rise to 40% in moderate to severely obese individuals. With the increasing incidence of obesity in the country NAFLD has become a growing problem. About two-third of adults are either overweight or obese, and about 9 million American children over age 6 are considered obese and same number are overweight.
Associated conditions:
NAFLD/NASH is associated with a metabolic complex characterized by diabetes mellitus, obesity, high blood pressure, high cholesterol/triglycerides (hyperlipidemia) and resistance to insulin.
Symptoms:
Most patients with NAFLD/NASH may not have any symptoms and in those that are symptomatic the manifestation are non-specific. Fatigue and occasional upper abdominal discomfort may be present in a small number of patients only. On examination liver may be enlarged in less than half of the patients. Most of the patients are between 40-60 years of age, but the disease is well described in children as well. Children are more prone to have symptoms of upper abdominal discomfort and pain as compared to the adults. In asymptomatic cases the finding of an abnormal liver chemistry (AST/ALT) at routine health check-up and absence of known cause of liver disease in an obese person is a strong indicator of the diagnosis of NAFLD/NASH.
Confirming the diagnosis of NAFLD/NASH:
Liver biopsy remains the gold standard but imaging of liver with ultrasound is a useful non invasive test.

Normal Liver cells without fat
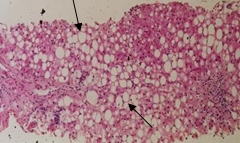
Fat deposits in Liver cells
Treatment of NAFLD/NASH involves modification of lifestyle, use of anti-oxidants, and avoidance of agents potentially toxic to the liver. Research is in progress to evaluate other medications that may selectively intervene at the mechanism that initiate the disease. A gradual weight reduction, abstinence from alcohol, better control of diabetes, and other concurrent illnesses are important to slow the progress of the disease. Patients should be followed closely for early detection of progressive liver injury or its complications including liver cancer.
IV. Acute Fulminant Hepatic Failure:
It is an acute catastrophic event with sudden onslaught of massive liver injury in a person who has had normal liver all along. The condition manifests with rapidly deteriorating liver function, progressive alteration in mental status leading to coma, deranged blood clotting and rapid onset of failure of kidneys, lungs and susceptibility to infection.
Causes of acute fulminant heptic Failure:
Majority of cases are due to virus infection or to drugs. Incidence of acute fulminant hepatitis in acute hepatitis A is less than 0.3%, in acute hepatitis B 1-4%, with hepatitis C it is very low. In one third of the cases no identifiable cause may be found. Amongst drugs Tylenol overdose is the most common cause. Other causes include liver failure in the last three months of pregnancy, a disease where abnormal amount of copper accumulates in liver (Wilson's disease) and mushroom poisoning. Urgent liver transplant is the only option in patient not showing signs of quick recovery.
V. Alcoholic Liver Disease:
Heavy drinking over a long period of time can take its toll on the liver. Alcohol produces three types of liver injury:
a. Fatty liver: there is abnormal and excess accumulation of fat in liver cells that interferes with its proper functioning.
b. Alcoholic hepatitis: Inflamed liver with liver injury.
c. Cirrhosis: Scarred liver with significant liver cell injury.
According to the Scientific Registry of Transplant Recipients, alcoholic liver disease was the third leading indication for liver transplantation in 2003 (26 percent of the transplant recipients in this category also were infected with hepatitis C).
If alcoholic liver disease is identified in an early stage like fatty liver and if the person stops drinking, it is possible that his or her condition could improve. However, these are two major "ifs," considering the often-silent nature of liver disease and the difficulty of breaking an addiction. As the liver disease advances to cirrhosis these patients require liver transplant like any other patients with cirrhosis of liver.
Patients with alcoholic liver disease must meet the following criteria to be considered for liver transplantation at University Hospital:
a. abstinence from alcohol use
b. ongoing participation in an alcohol treatment program or support group
c. presence of an adequate psychosocial support system.
These patients must enter a formal contract with the transplant team outlining the parameters of abstinence from alcohol use.
VI. Wilson's disease:
Normally, the liver helps the body rid itself of copper. In people with Wilson's disease, the gene responsible for this process is defective and copper builds up in the liver, the brain, and other organs. Over time, too much copper in the liver can lead to symptoms such as jaundice and swelling of the abdomen and, untreated, lead to acute liver failure, a need for liver transplantation, or death. Many patients, when diagnosed early on, respond well to the drugs that help remove copper from the bloodstream. They must take the medicine for the rest of their lives. There is an acute form of Wilson's disease in which the copper overload is swift and the organ damage is rapid . In patients with liver failure from wilson's disease liver transplantation is life saving.
VII. Hemochromatosis:
It is a disease of excess iron deposition in the liver and other organs of the body. Excess iron deposits in the liver damages the liver with destruction of liver cells and accumulation of scar leading to cirrhosis (scarred liver) that can not function. Hemochromatosis affects one in every 300 to 400 people. It is genetically inherited disease. The prevalence of the gene for hemochromatosis is not uncommon (10%) in people of North-Western European descent. To be affected by the disease person has to have acquired the gene from each of the parents. Family history and follow-up of immediate relatives of patients with hemochromatosis is important.
Symptoms usually develop between the ages of 40-60 years of age. Liver damage usually causes jaundice (yellowing of eyes and skin). Excess iron deposition in other organs may manifest as joint pain (arthritis), Diabetes (pancreas damage) skin pigmentation, heart abnormality (deposit of iron in heart), and hormonal problems (iron in pituitary gland).
Diagnosis is made by special blood tests to look for iron parameters, genetic markers, and measurement of iron from ma sample of liver tissue obtained by doing liver biopsy.
As the disease progresses to advances scarring (cirrhosis) other features of liver failure namely fluid accumulation, altered mental state, coagulation problems appear. Liver transplant is the only treatment option with progressive disease
Other Liver Diseases:
Alpha 1-Antitrypsin (AAT) Deficiency.
AAT (also known as alpha1 proteinase inhibitor) is a protein that is made primarily in the liver. This belongs to a group of proteins, which help prevent certain white blood cell enzymes (proteinases) from going beyond their regular infection-fighting functions to attack healthy body tissue. When the body doesn't make enough AAT, the lungs often don't work as efficiently (patients tend to develop emphysema) and the liver may be adversely affected, leading to cirrhosis. AAT deficiency is an inherited, condition, with two defective genes passed along–one by each parent. This rare deficiency affects fewer than 100,000 Americans.
Familial Amyloidosis Polyneuropathy.
This inherited disease, which occurs most often in people of Swedish and Portuguese descent, is a mutation of the transthyretin (TTR) molecule. Instead of the TTR protein being formed, an incorrect protein, amyloid, is produced. With this condition, amyloids are found throughout the body, destroying nerves and interfering with other organs. Neurological symptoms, low blood pressure, and muscle wasting are common manifestations of the disease, which can run a course of several years but has no cure. Because TTR is made in the liver, liver transplantation has been used as treatment.