Simulation Training

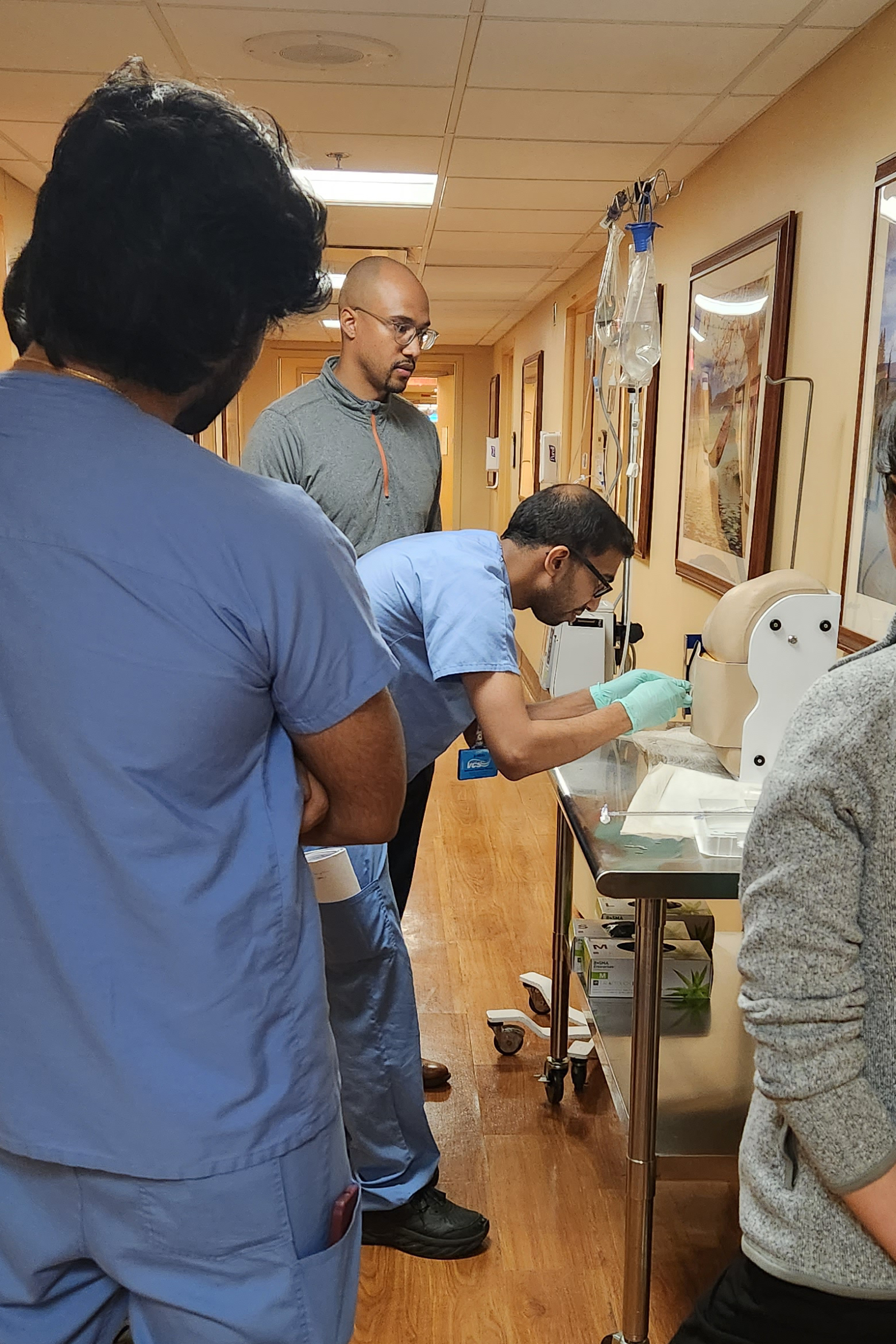
Our innovative Simulation curriculum allows for residents of all levels to gain hands-on experience in Codes and Early Response scenarios, as well as enhance proficiency in a variety of procedures. Our state of the art “Simulation Labs” at Cooperman Barnabas Medical Center and the VA mimic real life patient encounters, allowing for residents to work autonomously while being mentored and supervised in a controlled clinical environment. This type of unique, academic atmosphere grants learners a chance to receive tips and feedback on high-stress clinical scenarios while being in the safe space of the Sim Lab.
As part of this Simulation curriculum, residents have dedicated time allotted for them to complete at least 5 mandatory simulation exercises each year. Additionally, Chief Residents hold “open simulation hours” each week for residents desiring further practice. Residents also have dedicated time to explore the various procedures they will be expected to complete during their residency training. These procedures include ultrasound guided central lines, thoracentesis, paracentesis, arterial lines, intraosseous lines, lumbar punctures, intubations, arthrocentesis and many more.



Point of Care Ultrasound (POCUS)
All residents are taught the basics of POCUS during ICU rotations at University Hospital. Use of POCUS is integrated within bedside rounds, and all procedures performed in the ICU are under ultrasound guidance.
In 2019, a 2-week POCUS elective was implemented at the East Orange VA where residents have dedicated time to learn POCUS and practice their POCUS skills. Since 2018, 2-day POCUS courses are organized by NJMS faculty annually and all residents are invited to register.
Additionally in 2024, a procedures and POCUS elective was established at University Hospital, in which residents receive hands-on POCUS, vascular access, and bedside procedure training with Dr. Matassa and other general medicine proceduralists in the department.
Throughout their residency training, residents will also benefit from both observing and participating in interdisciplinary code blue training in which they can hone their BLS and ACLS training, as well as review videos of their own performance to improve.
We hold a yearly Procedure Night at the start of the academic year in which interns can learn directly from senior residents and Chiefs to gain exposure to procedural processes and supplies. The entire simulation curriculum has been created to ensure that all of our residents achieve mastery through rigorous assessment and practical experience.

