
Clinical Assignments
Our program is designed to train residents to hone their discriminating abilities, acquire clinical knowledge, and master the art of skillful, independent, and confident clinical decision-making by the time they graduate. The principal goals of our program include mastery of psychiatric evaluations and optimal management of both therapy and medication based approaches. Our residents are exposed to a variety of rotations across multiple sites, each offering different clinical experiences.
Residents rotate through the following sites which expose them to diverse patient populations across a multitude of socio-economic and cultural backgrounds.
- University Hospital (UH): Inpatient, outpatient, consultation and liaison, child and adolescent, and emergency psychiatric services
- VA Hospital at East Orange (EOVA) and at Lyons (LVA) campuses: Inpatient, general outpatient, addiction and PTSD clinics
- Rutgers University Behavioral Health Care (UBHC): General outpatient in a community setting
- Greystone Park Psychiatric Hospital (GPPH): Geriatric and forensics in a long term care setting
- Rutgers Newark College Counseling Center: Outpatient medication management and short-term therapy
- Jersey City Medical Center (JCMC): General outpatient in a community setting
University Hospital (UH)

UH is a separate, independent medical center with 519 licensed beds, an active medical staff of more than 600 and more than 3,100 employees. It is a regional resource for advanced care in a wide range of medical specialties. UH is home to northern New Jersey's Level-I Trauma Center and to specialty programs such as the Center for Liver Diseases and the Comprehensive Stroke Center.
VA Hospital at East Orange (EOVA)

VA Hospital at Lyons (LVA)

VA New Jersey Health Care System (VANJHCS) is a consolidated facility comprised of two main campuses, one in East Orange, and one in Lyons, 22 miles to the west of the East Orange Campus.
Primary care is the emphasis at the VANJHCS. Veterans are assigned their own health care providers who they see on a regular basis. Access to a wide variety of specialists is available through the primary providers. In addition to general medical, psychiatry, and long-term care, a full range of medical and surgical subspecialty care is provided to veterans of the VANJHCS. Residents have the opportunity to rotate through unique clinical opportunities such as the Veteran's PTSD clinic and the residential addictions rehabilitation program.
Greystone Park Psychiatric Hospital

Greystone Park Psychiatric Hospital is a 552-bed psychiatric hospital serving a designated New Jersey population. The new hospital opened on July 16, 2008 and is located in North Central New Jersey in Morris Plains.
Residents rotate in GPPH in their PGY-III and/or PGY-IV years. The main goal of this rotation is to learn skills in the treatment of chronically ill patients from a geriatric population. This facility also provides exposure to forensic psychiatry.
Rutgers Newark College Counseling Center

The counseling center serves the mental health needs of Rutgers Newark. The University's Newark branch encompasses over 13,000 students from over 100 different countries enrolled in one of 90 different programs of undergraduate, graduate, or professional studies. The center provides individual and group therapy, medication management, and connection to other wellness resources at the University.
Jersey City Medical Center (JCMC)

Jersey City Medical Center Behavioral Health Services is a mental health facility with inpatient, residential, and partial hospitalization treatment in addition to outpatient treatment. Residents rotate in JCMC in their PGY-III and/or PGY-IV years, with the primary goal of extended longitudinal care in the outpatient setting.
The Training
PGY-I: Getting Started
The maiden (intern) year consists of a half year rotation in psychiatry and a half year rotation in neurology and medicine, with an optional rotation in pediatrics. Some of the residents start with psychiatry; the others start with medicine or neurology.
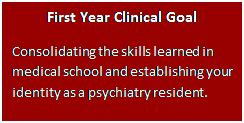 The Psychiatry rotation is an introduction to inpatient psychiatry, interviewing techniques and documentation. Residents rotate through UH and the VA.
The Psychiatry rotation is an introduction to inpatient psychiatry, interviewing techniques and documentation. Residents rotate through UH and the VA.
Residents ease into in-house calls with "buddy calls" where they are paired with senior residents for the first few calls. They learn history-taking, documentation, decision making, and system-based learning. After 1 or 2 buddy calls, each PGY-I starts "supervisory calls" where they take increasing responsibility in the calls in the presence of a senior resident. For most PGY-I residents, their first independent call comes after at least 5 buddy/supervisory calls. The maximum call duration on weekends is 12 hours. Each PGY-I resident gets one golden weekend per month with no calls. PGY-Is do not take independent calls for at least the first four weeks of their residency.
Neurology rotations are divided into two 4 week blocks with one block during PGY1 and the second during PGYII. The two months of Neurology provide the resident with knowledge of neurological evaluations and treatments. Neurology months take place at EOVA and UH which include a dedicated and fully accredited stroke service, an epilepsy service, a general neurology service and outpatient clinics. Neurology rotators are incorporate into the Neurology block schedule and join a team with a senior resident and a co-intern.
The Medicine rotation consists of four 4-week blocks. The focus is on the development of the basic medical skills and training necessary as a medical provider. The residents rotate at EOVA or UH. The training is divided between inpatient care, ambulatory care, and emergency medicine. Typically, there are no solo calls and a resident's team consists of one or two co-residents and a supervising senior medical resident.
PGY-II: Clinical Skills Advancement
The PGY-II year consists of rotations in EOVA, UH, HUMC and sometimes, UBHC. Residents are also introduced to Consultation-Liaison Psychiatry, Emergency Psychiatry and Outpatient Psychiatry.
Residents build on skills learned in PGY-I year and develop a more in depth approach to patient care.
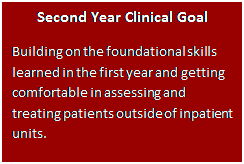 Residents learn Consultation-Liaison Psychiatry at UH and HUMC. This rotation teaches residents the fundamentals of psychiatric consultation in a primary care hospital setting. Both of the sites are busy with a high demand for psychiatric consultations. Residents learn to work with other teams and develop expertise in evaluating psychiatric symptoms in medically ill patients and to offer appropriate psychotherapeutic and psychopharmacologic interventions.
Residents learn Consultation-Liaison Psychiatry at UH and HUMC. This rotation teaches residents the fundamentals of psychiatric consultation in a primary care hospital setting. Both of the sites are busy with a high demand for psychiatric consultations. Residents learn to work with other teams and develop expertise in evaluating psychiatric symptoms in medically ill patients and to offer appropriate psychotherapeutic and psychopharmacologic interventions.
The Emergency Psychiatry experience is based in UH and can be a month-long or two-month long rotation. This is one of our busiest services and provides both a wide range and depth of exposure to various patient presentations. Here, PGY-II residents focus on rapid diagnostic assessments of adult and child patients with acute mental health issues. Residents work in collaboration with a multidisciplinary team under the direct supervision of an attending psychiatrist.
Full-time outpatient clinic experience starts in PGY-II for some residents. The focus is on evaluating and treating patients and the use of psychopharmacology and psychotherapy in outpatient settings.
Also, it is in the second year that all PGY-II residents begin psychotherapy training through the Lighthouse clinic. They are assigned a therapy supervisor and a patient caseload who they see in their own offices simulating outpatient private practice. They continue providing psychotherapy to these patients until they graduate.
PGY-II calls are less frequent than in the PGY-I year and provide an opportunity for expanded responsibilities and professional growth. Residents cover the inpatient psychiatry service and provide consultation services to the ER and to the general medical and surgical floors. PGY-II residents also provide supervision to PGY-I residents during the latter's buddy and supervisory calls.
PGY-III: Independence and Choosing a Specialty
The core focus for the PGY-III residents who started their longitudinal outpatient psychiatry experience in the second year is completing it. The core focus for the ones who did not is starting the longitudinal outpatient psychiatry experience.
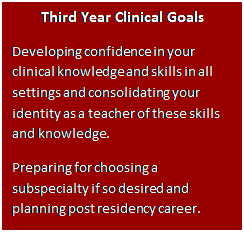 Outpatient exposure can be received in variety of clinical sites and settings including HUMC, VA, Rutgers College Counseling Center and UBHC. The site assignments for outpatient rotations take resident requests into consideration. The emphases during outpatient rotations are to ensure continuity of care and to develop a good therapeutic alliance with patients through longitudinal follow ups. Residents are provided with a balance of supervision and autonomy that will equip them to face clinical challenges in the future.
Outpatient exposure can be received in variety of clinical sites and settings including HUMC, VA, Rutgers College Counseling Center and UBHC. The site assignments for outpatient rotations take resident requests into consideration. The emphases during outpatient rotations are to ensure continuity of care and to develop a good therapeutic alliance with patients through longitudinal follow ups. Residents are provided with a balance of supervision and autonomy that will equip them to face clinical challenges in the future.
The PGY-III year can also include exposure to consultation and liaison psychiatry, emergency psychiatric services, college mental health, and inpatient experiences.
During this, year residents also continue with the Lighthouse clinic with a greater patient load and more responsibilities. Residents learn a wide variety of psychopharmacological interventions and receive extensive clinical training in CBT, psychodynamic, and supportive psychotherapies with supervision by senior psychotherapists.
PGY-III calls are much less frequent than in the PGY-I and PGY-II years with many more golden weekends. PGY-III residents also provide supervision to PGY-I residents during their supervisory and buddy calls.
PGY-IV: Professionalism, Uniqueness and Identity
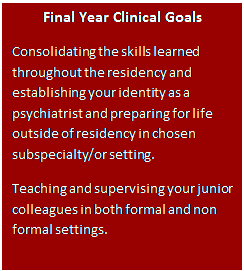 The PGY-IV year prepares residents for the next phase of their carrier. The cores of this year are mentored-training and academic work in individualized area(s) as residents develop expertise and readiness for independent psychiatric practice and directed professional growth. This is further amplified by the development of autonomy and identity.
The PGY-IV year prepares residents for the next phase of their carrier. The cores of this year are mentored-training and academic work in individualized area(s) as residents develop expertise and readiness for independent psychiatric practice and directed professional growth. This is further amplified by the development of autonomy and identity.
Each PGY-IV resident works with the program director to develop their clinical schedule. Usually, 6 months are dedicated to finishing any core requirements that may not have been completed. The remaining 6 months are used as a combination of elective and selective time providing each resident with an opportunity to define and pursue a concentrated focus. The elective time (2 months) may be used in clinical, research, teaching, or administrative settings. Most of the clinical sites/rotations are available to be used for the selective time (4 months).
During the PGY-IV year residents also continue with the Lighthouse clinic with a lower patient load but with greater focus on building their psychotherapy and psychopharmacological skills. Lighthouse clinic provides residents with the experience of working with a few patients for 3 years – preview of the real world experience of psychotherapy. Each PGY-IV resident also spends a few hours a week teaching and mentoring PGY-I residents.
There is no individual On-Call in PGY-IV. Each PGY-IV resident provides supervision to a PGY-I resident in a daytime supervisory call for a total of 6 supervisory calls per year.

